The Medical Record
Humans have been practicing medicine for thousands of years. While the physicians of the ancient past documented their theories, cases, and observations quite extensively, the individual medical record as we know it may have only been in existence a few hundred years. Starting in early modern England, the most comprehensive medical record contained a name, date, complaint, history, diagnosis, remedy/therapy and payment. They ranged from small pocketbooks to grand folios.
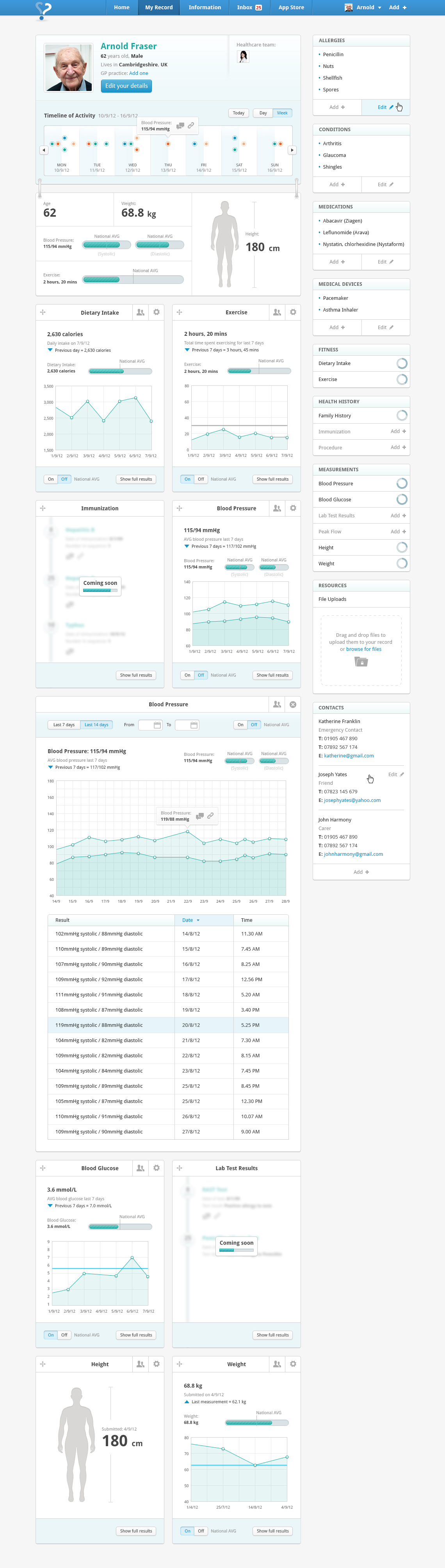
As the practice of medicine has evolved dramatically over the last three centuries, so did the medical record. The modern day medical record normally comprises basic patient data and demographics, medical history, medications and allergies, immunization, lab test results, radiology images, vital signs, personal statistics, and billing information. It provides information that is vital to providing quality patient care. The modern day medical record is also increasingly digital with the advent and widespread of Electronic Medical Records (EMR) software, which made it easier to provide better care, protect patient data, decrease processing times, set triggers and reminders, gain insights and conduct analyses.
The Patient
Despite the grand potential of health IT and the advances in EMR software, little progress has been made towards the portability of the medical record across healthcare organizations. There is a consensus around the vision and the importance of implementing a unified medical record system. This longitudinal collection of electronic health information about individual patients and populations has been commonly referred to as Electronic Health Records (EHRs). Some of the advantages of unified nation-wide or global EHRs would include:
- Improving healthcare services by facilitating movement of patients among healthcare providers, eliminating duplication, and reducing registration times.
- Collecting anonymous data on a macro level and gaining data-driven insights (big data, machine learning, and analytics), which can help in public health issues such as preventing infections, understanding genetic factors, predicting and controlling disease outbreaks, availability and capacity planning, enforcing best practices, research for new drugs, and even averting insurance fraud.
There are numerous challenges however that must be conquered to pave the way for a unified medical record, including non-standard data structures (medical record meta-data, charts, forms, taxonomy, reference ranges, language, etc.) which make data interoperability and comparability very difficult, in addition to privacy concerns, and lack of a central authority and enforcement on a national or international level.
Implementation
Many first world countries have had some significant success in launching such initiatives. In the US for instance, as is the case in Australia and the UK, the purer EHR model is evolving at the national level. To date, the IOM and the National Committee on Vital and Health Statistics (NCVHS) have focused primarily on the technical aspects of EHR implementation in the United States. Both have identified two core components in the project: first, building a national health information infrastructure and, second, establishing data interoperability and comparability for patient safety data. In order to achieve data interoperability and comparability, NCVHS and IOM have recommended the adoption of core standardized EHR terminologies (e.g., ICD-9 for diseases or symptoms, CPT-4 to code medical procedures, and services, and RxNorm for drug names and doses). Considerable development is also underway to standardize event taxonomy (e.g., adverse event or near-miss reporting using the College of American Pathologists’ SNOMED CT taxonomy) and to express knowledge representation such as clinical practice guidelines.
In the Middle East, Dubai was the first to launch such initiative through the Dubai Health Authority which announced last February the on-going development and deployment of a unique medical and health record system will integrate all 2,770 public and private health-care facilities in Dubai, providing a single electronic file for each resident. The system will eventually be linked to the National Unified Medical Record (NUMR) to be initiated by the Ministry of Health and Prevention in the UAE. The Electronic Medical Record (EMR) or Salama system will create one electronic record for patients across all public health hospitals, primary health centres and other facilities, while the Electronic Health Record (EHR) or NABIDH system will extend this medical record across all private hospitals, integrating medical records of the patients.
NABIDH (National Analysis and Backbone Integration for Dubai Health) which also means pulse in Arabic, will create big health data that will be used as an analytical tool in crisis management, management of disease outbreaks and also play a role in implementing preventive health care.
Health Information Management
At NVSSoft®, the imperative for the unified medical record is at the core of our product roadmap for our health information management system MedLogic eHIM®. As of its current release, MedLogic has already incorporated various elements that help in the implementation of unified electronic health records, such as:
- Providing the ability to achieve a single unified patient chart across multiple healthcare providers.
- Supporting the DICOM standard for unstructured images which can enable image-based analytics on a macro level.
- Using the XML standard to integrate and interlink its subsystems as well as third party systems in a multilayered environment.
- Linking with medical equipment and third party medical systems through the HL7 standard protocol.
- Supporting ICD-10 coding for medical diagnostics and procedures, manually and automatically.
- Supporting the JCI standard requirements when it comes to medical records
- Providing native iOS and Android applications.

We constantly follow the updates and advances in this domain to ensure that our technology fully supports the realization of a unified electronic health record that is portable across healthcare organizations, in addition to our mission of helping hospitals become fully paperless environments.